Details About
Hip Replacement
Restoring Mobility and Comfort
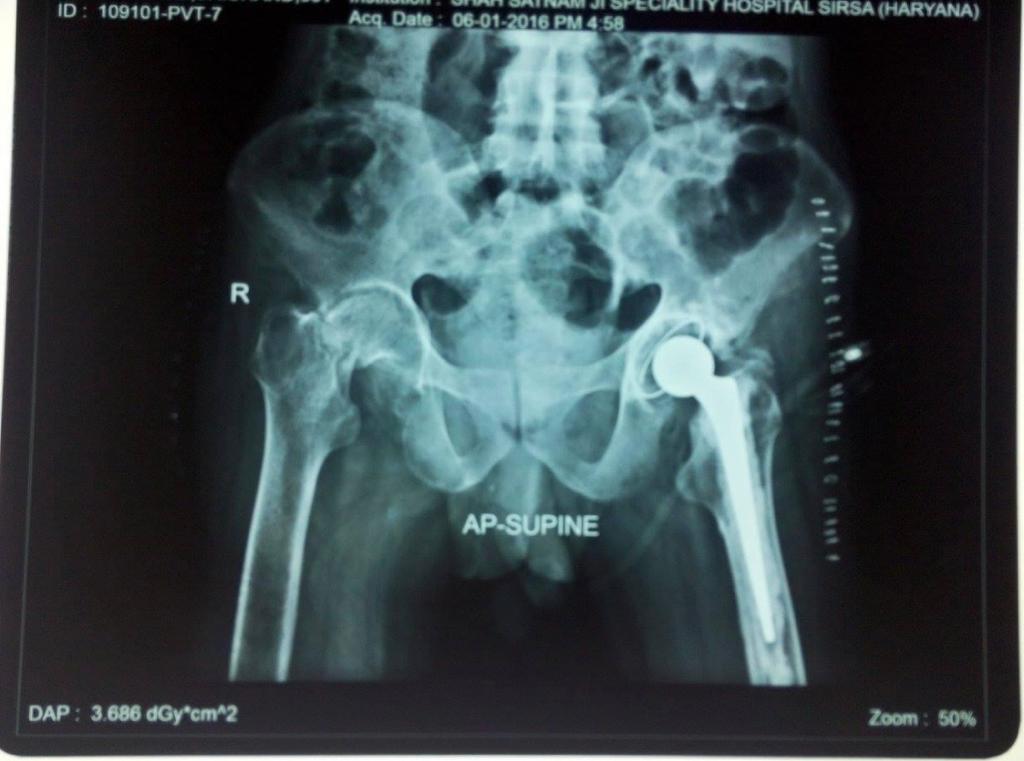
Hip replacement, medically termed hip arthroplasty, is a sophisticated surgical procedure meticulously designed to alleviate debilitating pain and restore functional independence in individuals afflicted by a damaged or severely arthritic hip joint. This transformative intervention becomes imperative when non-surgical remedies prove inadequate in mitigating pain and improving mobility. A comprehensive preoperative assessment is conducted, encompassing a meticulous review of the patient's medical history, a thorough physical examination, and the analysis of diagnostic imaging such as X-rays and MRIs. These evaluations serve to gauge both the patient's overall health and the extent of hip joint deterioration, helping the orthopedic surgeon determine the appropriateness of hip replacement.
The surgical approach to hip replacement can vary and is influenced by several factors, including the patient's specific condition, the surgeon's expertise, and the anatomical considerations. Surgical techniques range from the traditional posterior approach to the more minimally invasive anterior approach and lateral approach. Once the choice of surgical approach has been made, the procedure itself involves anesthesia, typically either general anesthesia or regional anesthesia such as a spinal or epidural block to numb the lower part of the body.
The surgical process commences with a carefully placed incision over the hip joint, which provides access to the compromised joint. The length and location of the incision depend on the chosen surgical approach. Once access is gained, the damaged or arthritic bone and cartilage within the hip joint are meticulously removed, creating space for the insertion of artificial hip components. These prosthetic components, including the femoral stem, acetabular cup, and other specialized parts, are precisely positioned and securely fixed within the joint. These components can be constructed from various materials, such as metal, ceramic, or high-density polyethylene, depending on the individual patient's needs and circumstances.
Following the successful placement of the artificial hip components, the incision is meticulously closed using sutures or staples, and appropriate dressings are applied to promote optimal healing. Postoperative care is characterized by close monitoring of the patient's vital signs and initial recovery in a designated area before transfer to a hospital room. Here, the patient's postoperative pain management, as well as the initiation of physical therapy, is of paramount importance. The early stages of rehabilitation are vital for regaining strength, range of motion, and overall stability in the newly replaced hip joint.
The journey towards full recovery can vary from patient to patient, but most individuals can typically return to light activities within a few weeks. As their strength and mobility continue to improve over the ensuing months, they gradually reintegrate into more demanding physical activities. Hip replacements have a well-documented track record of providing substantial pain relief and significant improvements in joint function. Many patients experience long-term benefits, with their artificial hips enduring for twenty years or more.
While hip replacement surgery is generally considered safe and effective, it is not without certain inherent risks and potential complications, including infection, blood clots, implant wear, or dislocation. The decision to undergo hip replacement should be made in consultation with a highly qualified orthopedic surgeon, taking into consideration the individual's specific medical history, lifestyle, and unique circumstances. Ultimately, hip replacement stands as a remarkable medical advancement, offering renewed hope, mobility, and a vastly improved quality of life to those suffering from the debilitating effects of hip joint disorders.
1. Preoperative Evaluation
The preoperative evaluation for hip replacement is a crucial step in determining the suitability of the procedure for an individual. It begins with a thorough assessment of the patient's medical history, including any underlying health conditions, previous surgeries, medications, and allergies. A physical examination is then conducted to evaluate the current status of the hip joint, assessing factors like range of motion, joint stability, and the presence of any deformities or abnormalities.
In addition to the clinical evaluation, diagnostic imaging studies such as X-rays and MRIs are often performed. X-rays provide detailed images of the hip joint, allowing the surgeon to assess the extent of joint degeneration, bone damage, and alignment issues. MRIs offer a more comprehensive view of the soft tissues surrounding the hip joint, helping to identify conditions like cartilage damage or labral tears. Collectively, this comprehensive evaluation guides the surgeon in making an informed decision regarding the necessity and appropriateness of hip replacement surgery for the patient, taking into account their overall health and the severity of hip joint issues.
2. Surgical Approach
The choice of surgical approach in hip replacement surgery plays a crucial role in the procedure's success and the patient's recovery. There are three primary approaches: the traditional posterior approach, the anterior approach, and the lateral approach. The selection of the approach is determined by several factors, including the patient's specific condition, the surgeon's expertise, and the patient's anatomical characteristics.
The traditional posterior approach involves making an incision at the back of the hip joint, allowing the surgeon to access the hip joint by moving muscles and soft tissues to the side. This approach provides good visibility and has been used for decades, making it a familiar choice for many surgeons. However, it may involve more muscle disruption, potentially leading to a longer recovery period and a higher risk of dislocation in the early postoperative phase.
The anterior approach, on the other hand, involves making an incision at the front of the hip joint. This approach is designed to minimize muscle disruption by following the natural muscle planes, potentially resulting in a quicker recovery with less pain. Surgeons who are skilled in this approach may choose it for certain patients, but it requires specialized training and equipment. The anterior approach is often favored for its potential benefits in terms of early postoperative mobility and reduced muscle trauma.
The lateral approach involves an incision on the side of the hip, which allows the surgeon to access the hip joint by moving muscles aside. This approach is less commonly used compared to the posterior and anterior approaches. It may be chosen in specific cases where the surgeon believes it offers advantages based on the patient's anatomy and condition.
In summary, the choice of surgical approach in hip replacement surgery is a complex decision that involves considering the patient's individual needs, the surgeon's expertise, and the potential benefits and risks associated with each approach. Patients should discuss their options thoroughly with their orthopedic surgeon to determine the most suitable approach for their hip replacement procedure.
3. Anesthesia
In hip replacement surgery, the choice of anesthesia is a critical decision that is carefully tailored to each patient's needs and the surgeon's preferences. Two primary options are commonly used: general anesthesia and regional anesthesia.
General anesthesia renders the patient completely unconscious throughout the surgical procedure. It induces a controlled state of unconsciousness, often through intravenous medications and inhaled gases. Under the influence of general anesthesia, the patient does not experience pain, awareness, or memory of the surgery. This allows the surgical team to work on the hip joint without causing discomfort or distress to the patient. General anesthesia is typically chosen when the surgical team needs the patient to be fully immobilized, ensuring precise control of the surgical site. It is also beneficial for patients who may have significant anxiety or fear associated with the procedure and prefer to be unaware of the surgical process.
In contrast, regional anesthesia, such as a spinal or epidural block, numbs only the lower half of the body, leaving the patient awake and alert during the procedure. A spinal block involves injecting anesthetic medication into the cerebrospinal fluid around the spinal cord, while an epidural block is administered into the epidural space outside the spinal cord. These techniques provide pain relief and muscle relaxation in the lower body without affecting consciousness. Regional anesthesia is often favored when the surgical team and patient want to minimize the risks and side effects associated with general anesthesia. It allows for a faster recovery after the surgery and can be an excellent option for patients who prefer to be aware of their surroundings during the procedure. The choice of anesthesia is made through a collaborative decision involving the patient, surgeon, and anesthesiologist, considering the patient's health, medical history, and individual preferences.
4. Incision
The incision is a pivotal step in hip replacement surgery as it provides the surgical team with access to the hip joint, enabling them to perform the necessary procedures and replace the damaged joint with artificial components. The precise placement, length, and location of the incision can vary, depending on the surgical approach chosen for the specific patient.
The choice of the incision length primarily hinges on the surgical approach employed. Traditional approaches, such as the posterior or lateral approaches, often involve slightly longer incisions, typically around 8 to 10 inches. These incisions may extend from the buttocks to the upper thigh, or they may be made on the side of the hip. Although these approaches offer adequate visibility of the hip joint, they may result in more post-operative pain and a longer recovery period due to the larger incision.
In contrast, modern minimally invasive techniques, like the anterior approach, use smaller incisions, usually around 3 to 4 inches in length. These incisions are typically made at the front of the hip, allowing for less disruption of muscles and tendons. The smaller incisions can lead to reduced post-operative pain, shorter recovery times, and fewer complications related to tissue damage. However, not all patients are candidates for minimally invasive approaches, as they may be more complex and require a specific patient anatomy.
The location of the incision also plays a significant role in the overall surgical process. The surgeon carefully selects the location to ensure the best access to the damaged hip joint while minimizing disruption to surrounding structures. This careful planning aims to protect critical blood vessels and nerves, reduce the risk of complications, and facilitate a successful surgical outcome.
Ultimately, the surgeon's experience and the patient's specific medical condition guide the decision regarding the incision. Regardless of the approach chosen, the incision is a crucial part of the procedure, as it provides the gateway to restoring mobility and relieving pain in individuals with debilitating hip joint conditions. Proper post-operative care and adherence to the surgeon's recommendations can help patients achieve the best possible results in their hip replacement journey.
5. Hip Joint Resurfacing
Hip joint resurfacing is a specialized surgical technique that may be recommended in specific cases as an alternative to a complete hip joint replacement. This approach involves the removal of damaged cartilage and the application of a metal prosthesis to cap the femoral head, preserving a significant portion of the patient's natural bone. The primary goal of hip resurfacing is to address the underlying issues causing pain and limited mobility in the hip joint while retaining as much of the patient's original bone structure as possible.
Hip resurfacing is typically considered for patients with specific hip conditions, including early-stage osteoarthritis or hip dysplasia. In these cases, the damage is often localized, and the femoral head remains relatively healthy, making it a suitable candidate for resurfacing. The preservation of the natural bone can provide potential advantages for the patient's long-term joint health and may offer more flexibility for future treatment options.
The success of hip resurfacing depends on several factors, including the extent and location of joint damage and the patient's individual anatomy. Not all patients are candidates for this procedure, and the decision to pursue hip resurfacing is typically made after careful evaluation by the orthopedic surgeon. During this evaluation, the surgeon considers the patient's specific condition, lifestyle, and long-term objectives for hip health.
The hip resurfacing procedure begins with the removal of the damaged cartilage and any arthritic surfaces of the hip joint. The femoral head is then capped with a metal prosthesis that closely matches the patient's natural anatomy. This metal cap is affixed to the femoral head, and a metal shell is placed in the acetabulum (the hip socket). The smooth surfaces of the metal components create a low-friction, durable joint, allowing for improved mobility and reduced pain.
One potential advantage of hip resurfacing is that it may lead to a lower risk of dislocation when compared to traditional hip replacements. It is also considered to be a bone-conserving option, meaning that if revision surgery is required in the future, the patient may have more viable bone stock available for a total hip replacement. However, hip resurfacing is not without its considerations, and patients should discuss the risks, benefits, and suitability of this procedure with their orthopedic surgeon.
As with any surgical procedure, the success of hip joint resurfacing depends on several factors, including patient adherence to post-operative care and rehabilitation. Patients typically undergo physical therapy to regain strength and mobility in the hip, with the goal of returning to their regular activities with reduced pain and improved hip function.
6. Removal Of Damaged Tissue
A critical step in hip replacement surgery is the removal of damaged or arthritic bone and cartilage within the hip joint. This process is essential to create the necessary space for the placement of artificial implants, which will restore the hip joint's function and alleviate pain.
The surgeon carefully excises the damaged tissues, which are often the source of discomfort and limited mobility for the patient. This step involves precision and skill, as it ensures that the artificial implant can be securely positioned within the joint. By removing the damaged bone and cartilage, the surgeon prepares a clean, stable environment for the new components.
This meticulous removal of the damaged tissue is a fundamental part of the procedure, as it directly impacts the success of the hip replacement surgery. It allows for the seamless integration of the artificial implant, which closely mimics the natural joint's structure and function.
Patients can expect that after the removal of damaged tissue, they will experience significant relief from pain and improved hip joint function. Post-operative care, including physical therapy, is typically required to aid in the recovery process, helping patients regain strength, mobility, and stability in their newly reconstructed hip joint.
As with any surgical procedure, the success of hip joint resurfacing depends on several factors, including patient adherence to post-operative care and rehabilitation. Patients typically undergo physical therapy to regain strength and mobility in the hip, with the goal of returning to their regular activities with reduced pain and improved hip function.
7. Implant Placement
Implant placement is a crucial phase in the hip replacement surgery, where the artificial hip components are meticulously positioned and securely fixed within the joint. These components typically consist of the femoral stem, acetabular cup, and any associated parts, each carefully chosen to match the patient's unique needs and anatomy.
The surgeon's skill and precision are paramount during this step, as the proper alignment and placement of these components are essential for the success of the procedure. The femoral stem, typically made of metal, is inserted into the hollowed femur to provide stability and support. The acetabular cup, which can be composed of materials like ceramic or high-density polyethylene, is implanted in the hip socket to recreate a smooth, low-friction joint surface.
The choice of implant materials may vary based on the patient's specific needs and the surgeon's expertise. These materials are selected for their durability and compatibility with the patient's lifestyle, aiming for long-lasting pain relief and improved joint function.
Once the artificial components are securely in place, they mimic the natural hip joint's structure and function, offering patients the potential for renewed mobility and a significant reduction in pain. The success of implant placement significantly contributes to the overall effectiveness of hip replacement surgery.
8. Closure
The closure of the incision marks the final step in the hip replacement surgery. After the artificial components are securely placed and the joint is restored to its intended structure, the surgical team meticulously closes the incision to ensure proper healing and minimize the risk of infection.
Depending on the surgical approach and the patient's specific needs, the incision may be sealed using sutures or staples. The choice of closure method is made with careful consideration of factors such as the patient's skin type, incision length, and the surgeon's preference.
Once the incision is closed, dressings are carefully applied to protect the surgical site and promote a clean, sterile environment for healing. These dressings are designed to minimize the risk of infection while allowing for adequate airflow to the incision.
The surgical team ensures that the incision is well-sealed to prevent any post-operative complications. Proper wound care and monitoring are crucial during the early stages of recovery to ensure that the incision heals as intended.
The closure of the incision represents the conclusion of the surgical procedure. From this point, the patient enters the recovery phase, with post-operative care, rehabilitation, and close medical supervision playing vital roles in the successful outcome of the hip replacement surgery.
9. Postoperative Care
After hip replacement surgery, postoperative care is a critical phase in the patient's journey towards recovery. Following the procedure, patients are closely monitored in a dedicated recovery area before being transferred to a hospital room. During this initial postoperative period, medical professionals ensure that the patient's condition is stable and that there are no immediate complications.
Pain management strategies are initiated to promote comfort and alleviate any surgical discomfort. Pain medications are carefully administered to control postoperative pain while minimizing side effects. Patients are encouraged to communicate their pain levels so that adjustments to the pain management plan can be made as needed.
In the early postoperative phase, measures are taken to prevent common complications such as deep vein thrombosis (DVT) and infections. Patients are often encouraged to engage in gentle leg exercises and wear compression stockings to promote circulation and reduce the risk of DVT.
The surgical wound is closely monitored for any signs of infection or other issues. Dressings are changed as necessary, and the incision site is kept clean to prevent infection. Patients are educated on how to care for their incision and advised on any signs of infection or complications to watch for.
Postoperative care is a collaborative effort between the medical team and the patient. Physical therapists often begin working with the patient to initiate early mobilization and help regain strength and mobility. The patient's involvement in their rehabilitation is crucial for a successful recovery and the restoration of optimal hip joint function.
10. Rehabilitation
Rehabilitation is an essential component of the recovery process following hip replacement surgery. It plays a pivotal role in helping patients regain strength, mobility, and stability in the hip joint, ultimately leading to an improved quality of life.
Physical therapists work closely with patients to create personalized rehabilitation plans tailored to their specific needs and abilities. These plans typically begin soon after surgery, with an initial focus on gentle exercises and mobility exercises that can be performed while minimizing strain on the healing hip.
As the patient progresses in their recovery, rehabilitation sessions become more intensive. Therapists guide patients through a range of exercises designed to increase muscle strength, improve joint flexibility, and enhance overall function. These exercises may include movements to strengthen the hip, knee, and surrounding muscles.
Rehabilitation also addresses activities of daily living (ADLs), helping patients relearn how to perform common tasks while protecting their hip joint. Therapists offer guidance on proper body mechanics, the use of assistive devices when necessary, and strategies for preventing falls or injuries.
The duration and intensity of rehabilitation vary depending on the patient's progress and specific surgical approach. Long-term success often hinges on a patient's commitment to the rehabilitation process and adherence to the prescribed exercises and activities.
11. Recovery Time
The duration of recovery following hip replacement surgery can vary from patient to patient, depending on several factors. While individual experiences may differ, a general timeline provides an overview of what most patients can expect during their recovery journey.
In the initial days following surgery, patients typically spend a short time in the hospital or a dedicated recovery facility. The primary focus during this period is on monitoring the patient's condition, managing pain, and preventing complications. The length of this hospital stay may range from a few days to a week.
Over the next several weeks, patients are gradually introduced to increased mobility and physical therapy. While they may require assistive devices like crutches or walkers at first, many patients can transition to walking unaided within a few weeks. Activities such as climbing stairs may also become more manageable.
Beyond the initial weeks, patients typically continue their rehabilitation and exercises at home. It is important to follow the guidance of the medical team and adhere to the recommended exercises for a successful recovery. Patients can often return to light activities and daily routines within a few weeks.
While the majority of patients experience significant improvements in the first few months, complete recovery and the ability to engage in more strenuous activities may take several months. Patients are encouraged to maintain regular follow-up appointments with their healthcare providers to monitor progress and address any concerns.
12. Long-Term Outcomes
Hip replacements are known for their ability to provide significant pain relief and improved joint function, leading to enhanced quality of life for patients. The long-term outcomes of hip replacement surgery are generally positive, with many patients experiencing lasting benefits.
Artificial hip components are designed for durability and longevity. While the lifespan of these implants can vary based on factors such as the patient's activity level and implant materials, many patients can expect their artificial hips to last for two decades or more. This means that most individuals can enjoy the benefits of their hip replacement for a considerable portion of their life.
Improved mobility and pain relief often result in an active and fulfilling lifestyle for patients who have undergone hip replacement surgery. They can engage in activities they may have had to avoid before the surgery, such as walking, cycling, swimming, and even low-impact sports. This renewed physical activity contributes to overall health and well-being.
It's important to maintain regular follow-up appointments with healthcare providers to monitor the condition of the artificial hip and address any concerns that may arise over time. While complications are rare, they can be addressed promptly if detected early, ensuring the continued success of the hip replacement.
In conclusion, hip replacement surgery offers patients the opportunity for long-term pain relief, enhanced mobility, and a better quality of life. With appropriate care and attention to their hip health, most individuals can enjoy the benefits of their new hip joint for many years, allowing them to stay active and engaged in the activities they love.